What is Bipolar Disorder?
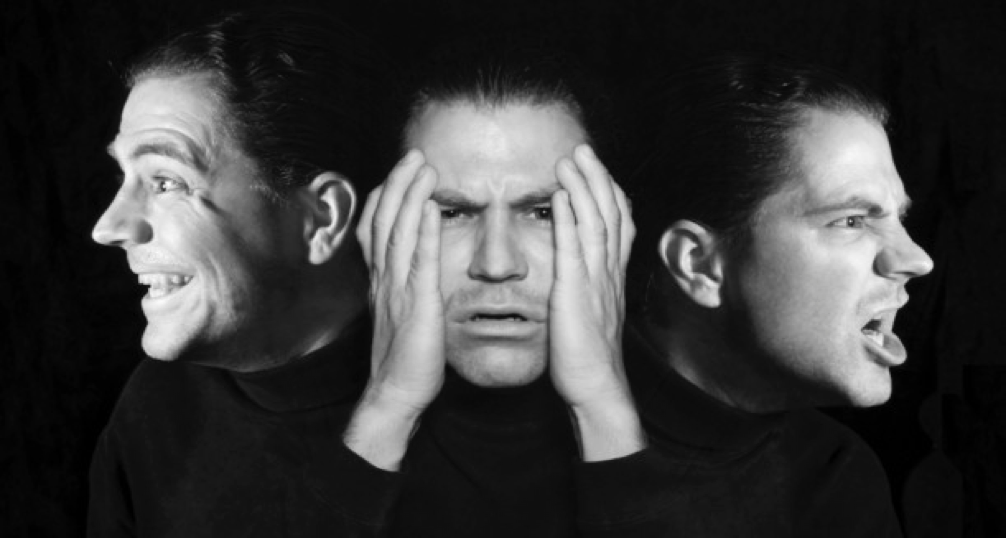
Bipolar disorder is a serious illness in the brain. It is also called manic-depressive illness or manic depression. People with bipolar disorder go through unusual mood changes. Sometimes they feel very happy and “up,” are much more energetic and active than usual. This is called a manic episode. Other times people with bipolar disorder feel very sad and “down,” have low energy and are much less active. This is called depression or a depressive episode. Bipolar disorder is not the same as normal ups and downs those without the disorder go through. With bipolar disorder the mood swings are more extreme and are accompanied by changes in sleep, energy level, and mental clarity. Bipolar symptoms are so strong that they can damage relationships and make it hard to go to school or keep a job. They can also be dangerous. Some people with bipolar disorder try to hurt themselves or attempt suicide.

Types of Bipolar Disorders
Bipolar I Disorder
This type of bipolar disorder is diagnosed when manic episodes last at least seven days and are accompanied by psychotic features, or the manic symptoms are severe enough to require immediate hospitalization to prevent harm to oneself or others. Depressive episodes, typically lasting at least two weeks, also often occur. A person may have manic episodes with some depressive features or depressive episodes with some manic features.
Bipolar II Disorder
This type of the disorder is diagnosed when a pattern of depressive episodes and hypomanic episodes is present, but the full-blown manic episodes of bipolar I do not occur. Hypomanic episodes have the same symptoms as manic episodes but are shorter in duration and less severe. Bipolar II disorder is more likely to be mistakenly diagnosed as depression.
Cyclothymic Disorder
Cyclothymia is a milder form of bipolar disorder that’s sometimes referred to as cyclothymic disorder. Both cyclothymia and bipolar disorder are characterized by extreme mood swings, from the highs of mania to the lows of depression, with short periods of neutral time in between. The difference lies in the intensity. People with bipolar disorder will experience clinically diagnosed mania and usually major depression, while people with cyclothymia have low-grade depression and mild symptoms of hypomania

Signs and Symptoms
Manic episodes may include symptoms such as high energy, reduced need for sleep, and loss of touch with reality. Depressive episodes may include symptoms such as low energy, low motivation, and loss of interest in daily activities. Mood episodes last days to months at a time and may also be associated with suicidal thoughts.
People may experience:
- Mood: mood swings, sadness, elevated mood, anger, anxiety, apathy, apprehension, euphoria, general discontent, guilt, hopelessness, loss of interest, or loss of interest or pleasure in activities Behavioral: irritability, risk taking behaviors, disorganized behavior, aggression, agitation, crying, excess desire for sex, hyperactivity, impulsivity, restlessness, or self-harm
- Cognitive: unwanted thoughts, delusion, lack of concentration, racing thoughts, or slowness in activity Psychological: depression, manic episode, agitated depression, or paranoia
- Sleep: difficulty falling asleep or excess sleepiness
- Weight: weight gain or weight loss
Diagnosis
Doctors have come a long way in fully understanding different moods in bipolar disorder and in making an accurate diagnosis. It wasn’t that long ago when bipolar disorder was confused with other disorders such as unipolar depression or with schizophrenia (a serious mental illness with symptoms of incoherent speech, delusions, and hallucinations). With the greater understanding of mental disorders today, doctors can identify the signs and symptoms of bipolar depression, hypomania, and mania. In most cases, they are able to treat the disorder effectively and safely with bipolar medications.
Most of us have become used to specialized blood tests or other laboratory measures to help our doctors make a more accurate diagnosis. However, most lab tests or imaging tests are not useful in diagnosing bipolar disorder. In fact, the most important diagnostic tool may be talking openly with the doctor about your mood swings, behaviors, and lifestyle habits. While a physical examination can reveal a patient’s overall state of health, the doctor must hear about the bipolar signs and symptoms from the patient in order to effectively diagnose and treat bipolar disorder.
Risk factors
- Genetics: Bipolar disorder tends to run in families. Children with a parent or sibling with the disorder have a higher chance of developing it than those without affected family members. Identical twins don’t have the same risk of developing the illness. It’s likely that genes and environment work together in the development of bipolar disorder.
- Environment: Sometimes a stressful event or major life change triggers a person’s bipolar disorder. Examples of possible triggers include the onset of a medical problem or the loss of a loved one. This kind of event can bring about a manic or depressive episode in people with bipolar disorder. Drug abuse might trigger bipolar disorder. An estimated 60 percent of individuals with bipolar disorder are dependent on drugs or alcohol. People with seasonal depression or anxiety disorders may also be at risk for developing bipolar disorder.
Medical Treatment
Anti-depressants and mood stabilizers are the most common medications.
Psychological Treatment
Psychological treatments are not an alternative to medication. However, when used in conjunction with the person’s medication certain psychological treatment programs have shown additional benefits, particularly in helping to prevent relapse, reduce symptoms, and improve daily functioning. Psychotherapy or “talk” therapy is an important part of treatment for bipolar disorder. During therapy, you can discuss feelings, thoughts, and behaviors that cause you problems. Talk therapy can help you understand and hopefully master any problems that hurt your ability to function well in your life and career. It also helps you stay on your medication. It can help you maintain a positive self-image.

Support Groups
Support groups also help people with bipolar disorder. You receive encouragement, learn coping skills, and share concerns. You may feel less isolated as a result. Family members and friends may also benefit from a support group. They can gain a better understanding of the illness, share their concerns, and learn how to best support loved ones with bipolar disorder.
How to Cope with Bipolar Disorder
- Establish routines: Regular sleep, eating, and activity appear to help people with bipolar disorder manage their moods.
- Identify symptoms: Even though the early warning signs of an approaching episode vary from person to person. Together with a psychiatrist you can identify what behavior changes signal the onset of an episode for you. It may be needing less sleep to feel rested, buying things you can’t afford or don’t need, becoming suddenly involved in religion, or new activities and interests.
- Adapt: This can help you avoid embarrassing behavior during manic episodes and set realistic goals for treatment. Your doctor can help you prepare for possible future episodes and manage fear about having more. A key part of adapting is to understand the types of stressors that might increase the risk for manic or depressive episodes and the lifestyle changes that can reduce them.
- Maintain a regular sleep pattern: Go to bed and wake up around the same times each day. Changes in sleep can disrupt the normal functioning of brain circuits involved in the processing of emotions, potentially triggering mood episodes.
- Do not use alcohol or street drugs: These substances can trigger or mimic mood episodes. They can also interfere with the effectiveness of medication.
- Emergency Plan: Despite your best efforts, there may be times when you experience a relapse into full-blown mania or severe depression. In crisis situations where your safety is at stake, your loved ones or doctor may have to take charge of your care. Such times can leave you feeling helpless and out of control, but having a crisis plan in place allows you to maintain some degree of responsibility for your own treatment.
Struggling with bipolar disorder? You are not alone.

